Addressing health & wellbeing of Allied Health Professionals
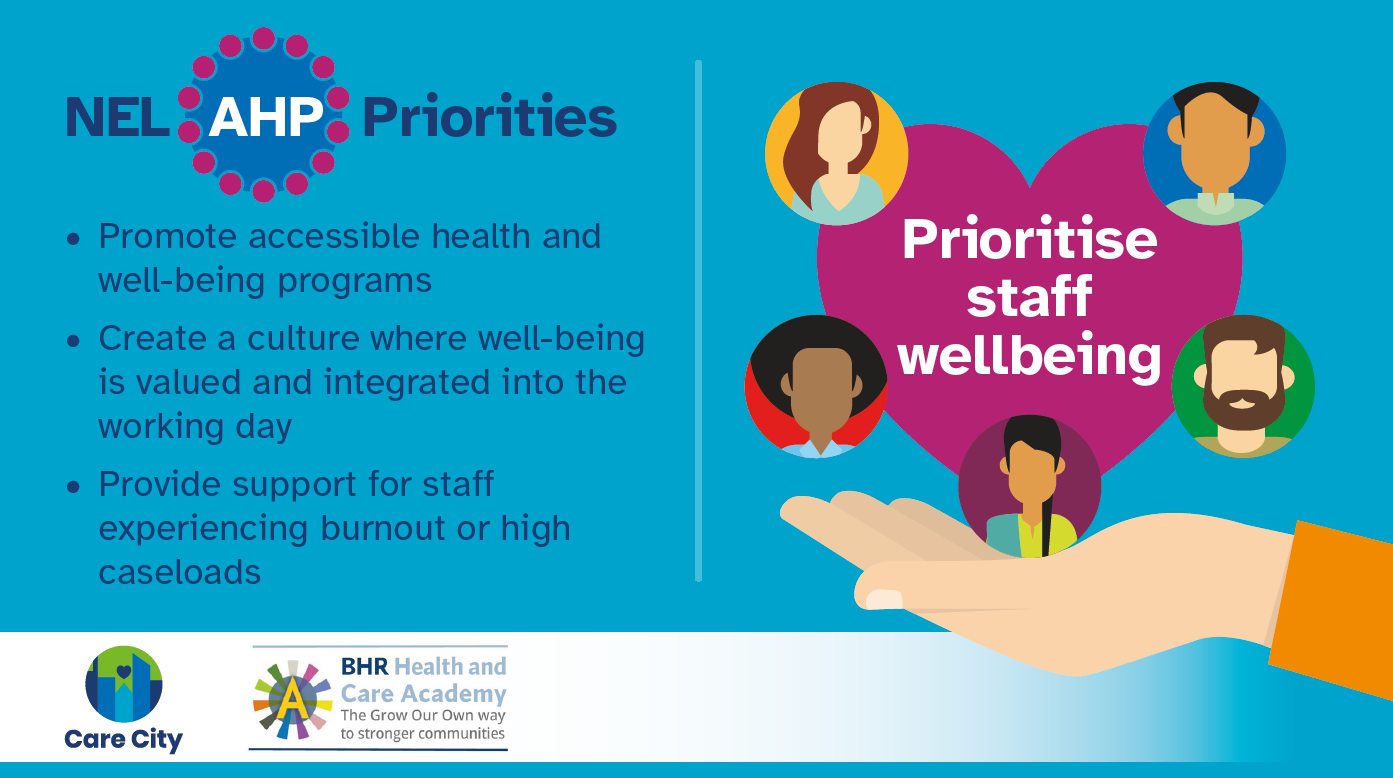
Our work with BHR Academy sought to address health and wellbeing of AHP staff during high patient demand.
The health and wellbeing of Allied Health Professionals (AHPs) plays a critical role in their ability to deliver high quality care to patients. However, amidst the numerous responsibilities and demands, AHPs often face challenges that can affect their personal health and well being.
Data from the BHR Academy Dashboard indicates an increase in sickness rates across the AHP workforce, with podiatrists experiencing the highest rates of sickness followed by radiographers, physiotherapists and occupational therapists.
We conducted a review of local and national organisational Health and Wellbeing offers and held interviews with Service Leads for Adult Community Services and Acute Teams, Children Services, Leads for OTs in Local Authorities and the Digital Therapeutics & Programme Lead for the Keeping WellNEL service – a North East London staff mental health and wellbeing hub which offered enhanced, health, wellbeing and psychological resilience support.
Our report details their thoughts and experiences about the health and wellbeing offers available to AHPs across Barking, Havering and Redbridge, reflections on why these offers might not be taken up and recommendations for next steps.
Headlines
Staff awareness of health and wellbeing offers
Health and wellbeing and the offers available are always discussed in team meetings, however the sheer number of wellbeing offers available could be a hindrance to awareness as it can becomes confusing.
Recommendation: Ensure that Health and Wellbeing offers are promoted and can be accessed, through a single channel to reduce confusing messaging.
Challenges to uptake
Accessing Health and Wellbeing offers can be challenging due to sessions being held during the day and not easily accessible to all staff members based on their location. And although staff members recognise the potential benefits of support, they believe their time is better spent in clinical contact, and tend to only access services reactively when there is a need.
Recommendation: Involving AHPs in the development and evaluation of health and wellbeing services can help ensure that the resources are tailored to their specific needs and preferences. AHPs on the ground should have a voice in shaping services to enhance their effectiveness and accessibility
Staffing and staff pressure
Pressures can be attributed to staff shortages, large volume waiting lists, and an increasing BHR population and historical staffing levels and can negatively impact staff well-being, potentially leading to higher sickness rates, burnout, decreased job satisfaction, and poor retention.
Recommendation: It’s crucial to recognise that the burden on AHP teams is a result of systemic issues within the health and care system, rather than individual shortcomings. This perspective shift will be necessary in addressing the experience of waiting list pressures and their prioritisation over personal wellbeing and accessing support. An improved understanding of the whole health and care system (through bringing together commissioners, health and care staff to discuss their roles and shared challenges) would support this.
Staff would rather get waiting lists down than look after themselves
Service Lead, Interviewee
We’ve also been talking to BHR AHP service leads to capture their perspectives of the challenges facing AHPs locally & ideas to support future workforce developments. Read the findings of our conversations here.



